Whether you have type 1 diabetes or type 2 diabetes, managing your blood sugar level is key. The higher your blood sugar level, the higher your risk of:
- Tooth decay (cavities). Your mouth naturally contains many types of bacteria. When starches and sugars in food and beverages interact with these bacteria, a sticky film known as plaque forms on your teeth. The acids in plaque attack the hard, outer surface of your teeth (enamel). This can lead to cavities. The higher your blood sugar level, the greater the supply of sugars and starches — and the more acid wearing away at your teeth.
- Early gum disease (gingivitis). Diabetes reduces your ability to fight bacteria. If you don't remove plaque with regular brushing and flossing, it hardens under your gumline into a substance called tartar (calculus). The longer plaque and tartar remain on your teeth, the more they irritate the gum tissue. In time, your gums become swollen and bleed easily. This is gingivitis.
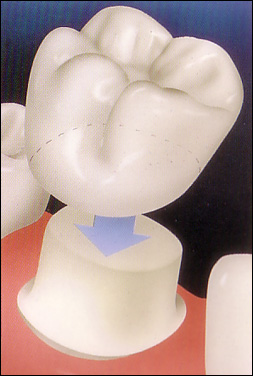
- Advanced gum disease (periodontitis). Left untreated, gingivitis can lead to a more serious infection called periodontitis, which destroys the gum tissue and bone that support your teeth. Eventually, periodontitis causes your gums to pull away from your teeth and your teeth to loosen and even fall out. Periodontitis tends to be more severe among people who have diabetes because diabetes lowers the ability to resist infection and slows healing. An infection such as periodontitis may also cause your blood sugar level to rise, which makes your diabetes more difficult to control. Preventing and treating periodontitis can help improve blood sugar control.
To help prevent damage to your teeth and gums, take diabetes and dental care seriously:
- Make a commitment to managing your diabetes. Monitor your blood sugar level, and follow your doctor's instructions for keeping your blood sugar level within your target range.
- Brush your teeth at least twice a day. Brush in the morning, at night and, ideally, after meals and snacks. Use a soft-bristled toothbrush and toothpaste that contains fluoride. Avoid vigorous or harsh scrubbing, which can irritate your gums. Consider using an electric toothbrush.
- Floss your teeth at least once a day. Flossing helps remove plaque between your teeth and under your gumline.
- Schedule regular dental cleanings. Visit your dentist at least twice a year for professional cleanings.
- Make sure your dentist knows you have diabetes. Every time you visit your dentist, remind him or her that you have diabetes. Make sure your dentist has contact information for your doctor who helps you manage your diabetes.
- Look for early signs of gum disease. Report any signs of gum disease including redness, swelling and bleeding gums to your dentist. Also mention any other signs and symptoms, such as dry mouth, loose teeth or mouth pain.
- Don't smoke. Smoking increases the risk of serious diabetes complications, including gum disease. If you smoke, ask your doctor about options to help you quit.
Managing diabetes is a lifelong commitment, and that includes proper dental care. Your efforts will be rewarded with a lifetime of healthy teeth and gums.